Created 12.04.2020
Health and Healthcare
Health and Healthy Lifestyle
Health is a state of physical, mental and social well-being, the absence of disease. More and more, it is becoming maintained and improved through the advancement and application of health science, but also through the efforts and intelligent lifestyle choices.Key factors to influence health include physical environment, especially pollution; culture, education and literacy; income, social status and environment and working conditions; biology, genetics and child development; and health policy and healthcare service availability. Lifestyle is the most important factor for Western countries, bad personal decisions lead to diseases of affluence. The environment, on the other hand, is a key factor in poor developing contries, where people have little control over the quality of food, water and air. The third factor is genetic make-up, which is thought to influence about 10% of physical and mental health. In the end, doctors are able to influence about 5% of all medical conditions, the rest requires mainly changes in lifestyle and living conditions.
The World Health Organization (WHO) is a specializes agency of the United Nations responsible for international public health. It advocates for universal healthcare, monitors public health risks, coordinated responses to health emergencies and promotes human well being. It also provide technical assistance to countries, sets international health standards and guidelines, and collects data on global health issues. The agency played a leading role in the eradication of smallpox, the near-eradication of polio and the development of an Ebola vaccine.
Healthy Lifestyle
To stay healthy, people should take care of themselves physically, mentally and socially. This means people should do their best to have a healthy lifestyle, live in a healthy area and have healthy relationships.Healthy food and water are the main factors of healthy lifestyle, including the amount of food and water consumed. Eating fresh fruit and vegetables and drinking enough clean water is the best way to maintain healthy body weight. A healthy diet should have all the important nutrients, people should avoid processed food, food additives and dietary supplements. Also, people should drink clean water moderately, when they are thirsty or when their lips are dry.
Exercising is another key factor for staying healthy in the Western society. People used to be more active in the past and it is important to maintain physical fitness in order to stay healthy. Sport leads to overall wellness, because many individuals choose to exercise outdoors and socialize during fitness activities. For people with a sedentary lifestyle, even small exercise such as housework or walking can make a difference and reduce the risk of cardiovascular problems and stress.
Sleep is another important factor of health. Humans restore themselves during sleep, when the metabolic rates decrease and metabolic waste products are removed from the body. Studies suggest that sleep deprivation may impair the abily to heal and it affects the immune system.
To achieve a healthy lifestyle, people should make relatively easy and small changes. Drastic changes and measures often lead to failure and can even worsen the lifestyle of person. It is important to stay positive and motivated, because mental well being is also important. People should also try to socialise with others who are trying to live healthier or who already have a healthy lifestyle, a supportive community can have a very pocitive impact.
Unhealthy Lifestyle
An unhealthy lifestyle is when a person engages in activities that are detrimental to health.Again, food is the main factor, an unhealthy diet means that a person is eating too much, too little or choosing unhealthy food. Obesity is a big problem in developed countries, about 12% of adults worldwide are obese. Unhealthy food includes junk food, highly processed food, food which includes too many additives and food which contains too little nutrients. Eating disorders include anorexia, bulimia and binge eating, and at some point in life over 10% of people worldwide have this problem.
Up to 2 billion people lack safe drinking water, which causes 30 thousand deaths every week. More poeple die from unsafe water than from war. In developed countries, overhydration is becoming a problem. When drinking too much, water can become toxic to the body and even cause death. About 4% of adults are alcoholis and about 3,3 million people die every year because of alcohol consumption.
Substance abuse is another worldwide problem, with about 5% of people using illicit substances, more than 300 thousand deaths are caused by substance use disorders. The WHO named tobacco use as the world's single greatest preventable cause of deaths, more than a billion people use tobacco and it causes more than 8 million deaths each year.
The condition of not having enough sleep is called sleep deprivation, it can be both chronic and acute. It can worsen any medical condition and can even lead to psychosis, it affects the brain's activity and function. Also, microsleeps can be very dangerous, especially when driving.
Chronic stress puts a strain on the human body for a long time and can have a serious impact on health. It may lead to high blood pressure and heart disease, diabetes, damage to muscle tissue, supression of the immune system, stopping of growth and damage to mental health. All this leads to further bad choices in lifestyle which makes the condition even worse.
Promiscuity is the practise of engaging in sexual activity frequently with different partners. There are different standards in different cultures but it is an important question in the epidemiology of sesually transmitted diseases. More than 30 different bacteria, viruses and parasites can be transmitted through sexual activity, including HIV and syphilis. More than a billion people have STIs, about 750 thousand people die of AIDS and another about 105 thousand of other STIs every year.
Healthcare
Healthcare is the maintenance or improvement of health via prevention, diagnosis, treatment, recovery or cure of disease or injury. It is delivered by health professionals, physicians, nurses and other specialists. It includes primary, secondary and tertiary care and public health. Access to healthcare may vary across countries. Healthcare systems are organizations established to meet the health needs of targeted populations.Health insurance covers the risk of a person incurring medical expenses. It can provide coverage for the payments of benefits as a result of sickness or injury. There are many ways how this is organized, many countries have a social health insurance system and a mandatory insurance.
Sick leave, also called paid sick days or sick pay, is time off from work for health and safety reasons. It guarantees paid time off to stay home when sick or caring for sick family members. It is a statutory requirement in many nations.
A sick note, sometimes called a medical certificate, is a written statement from a physician that serves as documentation that an employee is unfit for work or as evidence of a health condition. It can be required to obtain health benefits from an employer and for tax purposes. Also, specific health criteria or medical history are required for certain jobs.
Healthcare can be subdivided into primary, secondary, tertiary and sometimes even quaternary care.
Primary care is the work of health professionals who act as a first point of consultation. It involves the widest scope of healthcare for all patients. A primary care practitioner must possess a wide breadth of knowledge in many areas. It is the day-to-day healthcare given to all patients in the healthcare system. Primary care physicians are sometimes referred to as general practitioners or family doctors.
Secondary care includes acute care, a necessary treatment for a short period of time because of serious health conditions. It is often found in hospitals, especially emergency departments. Depending on the situation, patients may be required to see a primary care provider for a referral before they can access secondary care.
Tertiary care is specialized consultative health care, usually for inpatients or on referral. It is given in a facility that has personnell and facilities for advanced medical investigation and treatment, for example cancer management, neurosurgery and severe burns treatment.
Quaternary care is sometimes used to describe advanced levels of medicine which are not widely accessed. Experimental medicine and uncommon diagnostic or surgical procedures are offered in a limited number.
Hospital
A hospital is a health care institution providing patient treatment with specialized medical and nursing staff and medical equipment.The most common are general hospitals and district hospitals, which are the major health care facilities in the region. These hospitals typically have an emergency department to treat urgent health problems, a large number of beds for intensive care and additional beds for patients who need long-term care. A clinic is usually a medical facility smaller than a hospital, some can be highly specialized and some are polyclinics that provide general treatments.
On the other hand, there are specialized hospitals such as trauma centres, rehabilitation hospitals, children's hospitals, geriatric hospitals, and hospitals for dealing with specific medical needs. Thanks to their specialized staff and equipment, these can reduce health care costs compared to general hospitals.
Teaching hospitals and university hospitals combine assistance to people with teaching to medical students and nurses and it is usually involved in medical research. Students included in these programs usually have several years of intership.
Hospitals consist of departments, traditionally called wards. A large hospital consists of many clinical departments, but most hospitals have an ER (emergency room) and several other inpatient departments. Some hospitals may also have specialized units such as maternity ward or ICU (intensive care unit). Common support units include pharmacy, pathology and radiology.
Many hospitals also have specialized acute services, such as a trauma centre, burn unit, surgery and urgent care. There are also psychiatric hospitals, sometimes called asylums, and mental health units, which are hospitals and wards specializing in the treatment of serious mental disorders.
An outpatient department is a department for patients who stay in the hospital for less than 24 hours. Patients go there for their treatment, therapy and sometimes minor surgery, this provided care is called ambulatory care. These departments are usually located on the ground floor or in an easily accesible building. There is usually a reception, a waiting room and an admission room or consulting room. Some specialized departments have outpatient units for patient checkups.
An inpatient department, sometimes calles clinical departments, can sometimes be further separated into several wards and units. There, patients are admitted to stay overnight for treatment, this can last from 24 hours to an indeterminate time, from days to sometimes until death. Treatment provided is called inpatient care. The admission to the hospital involves the production of an admission note, the leaving of the hospital is officially termed discharge and it involves a corresponding discharge note. These departments include rooms for patients, day rooms, bathrooms and kitchenettes, and can provide also education for children and occupational therapy. Some hospitals have chronic treatment units such as psychiatry wards, rehabilitation services and physical therapy departments.
The ER (Emergency Room), also called accidents & emergency, emergency department or casualty department, is a medical treatment facility specializing in emergency medicine. It provides acute care of patients who come without prior appointment, by their own means or by an ambulance. Due to the unplanned nature of the patient attendance the department must provide initial treatment for a broad spectrum of illnesses and injuries, of which some may be life-threatening and require immediate attention.
The ICU (Intensive Care Unit), also called intensive therapy, intensive treatment or critical care unit, is a special department that provides intensive tretment medicine, to patients with severe and life-threatening illnesses and injuries. These patients require constant and close monitoring and support from specialist equipment and medications in order to ensure normal bodily functions. It is staffed by highly trained doctors and nurses who specialize in caring for critically ill patients. Because of this, it has a higher staff-to-patient ratio and acess to advanced medical resources and equipment that is not routinely available elsewhere.
Auxiliary services are provided by departments of anesthesiology, radiology, blood transfusion centres, specialized laboratories and tissue banks. Emergency medical services, also called ambulance services or paramedic services, sometimes also rescue squad or ambulance corps, treat illnesses and injuries that require urgent medical response, providing out-of-hospital treatment and transport to definitive care. Air medical services move patients from accident scenes to healthcare facillities, usually via helicopter. Personnel, the flight crew, provide critical care to patients during evacuation or rescue.
Support units provide additional services, such a dispensary or a pharmacy. On the non-medical side, there are records departments, release of information departments, information managements, clinical engineering (biomed), facilities management, plant operations or maintenance, dining services and security departments.
A planned admission depends on many factors, including the importance of the treatment and the length of the waiting list of patients that also need it. Before, a genereal practitioner usually sends the patient to a specialist who assesses the patient's condition and sometimes recommends further tests. Depending on the urgency, the patient is then admitted to the hospital for planned treatment or surgery. Sometimes, patients are admitted without any previous appointments because of an emergency or a life-threatening condition.
All patients have to fill in the patient's record, also called medical record or medical chart. An admission note is the part that documents the patient's initial status, reason for being admitted for inpatient care and the initial instructions for care. The medical record consists of general information about the patient (name, date of birth, gender, contact person) and his health (allergies, medication and medical history) and also the name of his general practitioner. Before the patient is discharged from the hospital, doctors consider his current state, place of residence and the support available. The inpatient care is formally ended by a discharge note. Sometimes, patients are further monitored by follow-up appointments after the discharge.
The act of performing surgery is also called a surgical procedure or operation and a surgeon is a person who practices surgery. A surgical team is made up of a surgeon, surgeon's assistant, anesthetist, circulating nurse and surgical technologist.
Elective surgery is done to correct a non-life-threatening condition and it is carried out at the patient's request. A semi-elective surgery must be done to avoid permanent disability or death, but can be postponed for a short time. Emergency surgery must be done promptly to save life or functional capacity. Incision is a cut made into the body during surgery.
Cosmetic surgery is done to subjectively improve the appearance of a normal structure. Reconstruction surgery involves reconstruction of an injured, mutilated or deformed part of the body (-oplasty and -rraphy).
Amputation involves cutting off a body part. Resections and excisions are the cutting out of a whole or partial removal of an organ or body part (-ectomy and -otomy). Transplant surgery is the replacement of an organ or body part by insertion of another from a donor.
Minimally-invasive surgery involves smaller outer incisions to insert miniaturized instruments, such as in laparoscopic surgery (-oscopy). An open surgical procedure requires a large incision to access the area of interest (-ostomy).
A medical divice or medical equipment is any device intended to be used for medical purposes. In emergency situations, it can be an everyday object. In other cases, they must be proved safe and effective before they can be used. The design of medical devices constitutes a major segment of the field of biomedical engineering. Medical equipment is designed to aid in the diagnosis and for monitoring or treatment of medical conditions.
Treatment equipment includes infusion pumps, medical lasers and surgical machines. Life support equipment is used to maintain patient bodily functions and includes ventilators, incubators and anesthetic and dialysis machines. Medical monitors allow medical staff to measure patient medical state, such ass vital signs, ECG, EEG and blood pressure. Diagnostic equipment includes medical imaging machines, such as ultrasound, MRI machines (magnetic resonance imaging), PET (positron emission tomography) and CT scanners (computed tomography), TI (tactile imaging), IRT (thermal imaging - infrared telescope) and X-ray machines.
Hospital Staff
Hospitals are staffed by professional physicians, surgeons, nurses and allied health practitioners. Many units have both a nursing and a medical director that serve as administrators for their respective disciplines within that specialty. For both doctors and nurses, the names of their position in their medical career can differ in different countries.The Hippocratic Oath is taken by all doctors of medicine. The new physician swears to uphold specific ethical standards. The original oath was written between the 5th and 3rd century BC and is traditionally attributed to Hippocrates.
The Nightingale Pledge is a modified version of the Hippocratic Oath. It is a statement of ethic and principles of the nursing profession, but is is usually used only in the US.
 The United States of America follow different stages of qualification and use different terminology than the UK.
The United States of America follow different stages of qualification and use different terminology than the UK.In the US, physicians have the title of MD (Doctor of Medicine) and the term physician means either a specialist in internal medicine or any specialist. Doctors who work primarily in hospitals are called hospitalists. The US has the highest paid general practitioners in the world and second-highest paid specialists.
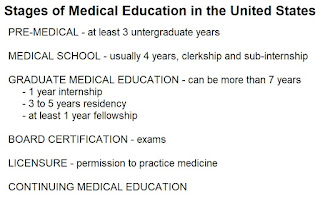
The US medical degrees are classified as secondary entry degrees and applicants have to complete at least 3 years of undergraduate pre-medical courses at the university level. The medical course lasts four years, two are pre-clinical and two are clinical, meaning students have clerkships in teaching hospitals, they are student doctors. During the last year, the studentshave a sub-internship, also called an acting internship, when the rotate in different wards and hospitals. Then, students apply for postgraduate residency in their chosen field of specialization.
Graduate medical education starts with a one year long internship, the minimum training requirement for obtaining a general license, they still require supervision. After that, students enter postgraduate training to become fully qualified. There are residency training programs, where each specialty has its own program and length from 3 to 5 years. The physicians and surgeons are called residents, house officers, registrars or trainees.
Those who completed the residency are called attending physicians. They then obtain an unrestricted license to practise medicine. In teaching hospitals, their team includes medical students at various stages of education who are supervised by them.
A fellowship is a formal, full-time training program that focuses on a particular area within the specialty. Many highly specialized fields require formal training beyond residency. The participants are called fellows, they have completed their residency and are certified in their basic specialty. A fellowship lasts from one to three years and usually has a research component.
All physicians must pass an exam in their specialty to become board certified. A medical license permits a person to practise medicine. Continuing medical education is designed for practicing physicians which can be required to maintain a license. It helps doctors to maintain competence and learn about new and developing areas in their field.
Patients are admitted to hospital under the care of the most appropriate staff specialist, also called the senior consultant, who develops a treatment plan for the more junior doctors. These specialists are extensively trained in one field, for example a cadriologist or a neurosurgeon. The specialists are on the ward only during rounds, while there should always be a junior doctor available. The attending physician is the leader of a team of doctors, he is responsible for the decisions. This doctor can be a hospitalist trained in internal medicine, a surgeon or a specialist.
In the United Kingdom, the medical career grades are defined by the NHS (National Health Service) and the terms are also used in Ireland and Australia. The NHS modernised the medical training programme in 2005. All leading British medical schools are state-funded and courses generally last four to six years.
Medical school starts with two years of pre-clinical training and two or three years of clinical training at a teaching hospital. After successful completion of clinical training, a student graduates as a Bachelor of Medicine. After graduation, medical students enter paid employment as a foundation house officer to complete their first year of foundation trainig. They, they have a year of supervised work to obtain a full registration.
Some students spend one or two more years at medical school studying for and intercalated degree. It is an extra qualification and depends on the university. Some students can earn a second bachelor's degree and some students may gain a master's degree in their fourth year of study. At the end of study courses, students may participate in research related masters and academic doctorates.
After medical school, junior doctors enter the two-year long Foundation Programme and then they can specialize in one field. To become a GP (general practitioner), a doctor must complete an 18 months-long course in a variety of hospital specialities and another 18 months in the General Practise Specialty Registrar. Hospital doctors have to take exams to become specialty registrars and eventually consultants. The highest level in speciality is the Certificate of Completion of Training. Then, doctors can complete higher degrees to become MD with a at least two-year full-time research course or PhD with a at least three-year full-time research course. Continuing medical education is now mandatory for all doctors.
A foundation doctor, also called a house officer, is a junior doctor undertaking the two-year long postgraduate Foundation Programme. This is compulsory for all newly qualified medical practitioners. The purpose is to gain experience in a series of posts in a variety of specialties and healthcare settings. A foundation doctor has a provisional registration with the General Medical Council. It is equivalent to an internship in other countries.
A specialty registrar works in a three-year specialty training programme. It is known as a training grade as they are supervised by senior doctors. This ensures necessary experience and qualification to be placed on the Genneral Medical Council's Specialist Register. Completing the course is awarded by a Certificate of Completion of Training.
A speciality doctor, called housemen, staff grade or middle grade by the old system, are appointed to a permanent position after at least 6 years of experience. Their main duties are ward rounds, supervision of junior doctors, emergency operating and serving hospital shifts in outpatient departments.
A consultant is a senior physician or surgen in a hospital, with a completed specialist training. They have the ultimate responsibility for the care of the patients and they are on the Specialist Register. They lead a team of doctors in training.
A head physician, also called chief physician, senior consultant, or chief of medicine, is a senior management position at a hospital. They are in charge of medical matters and superior to all other doctors. Mostly, they are the most experienced doctors and they may be in charge of other professional groups and areas as well.
Department of Nursing
Nursing is a profession within the healthcare sector focused on the care of individuals, so they may recover optimal health and quality of life. Nurses practice in many specialties with differing levels of prescription authority. Nurses develop a plan of care, working collaboratively with physicians, therapists, other team members and the patient and his family. Nurses also help coordinate the patient care performed by other members of the healthcare team.
Nurses are responsible for patient care, the administer medicine and give injections, take blood, urine, temperature, pulse and blood pressure. They are in charge of bed making, changing of surgical dressing, patient washing, doing round and assisting doctors. The job demands great patience, responsibility and a lot of work.
In the United States, nursing is provided by several levels of professional staff.
A certified nursing assistant has a short vocational course in nursing. They are trained to perform a limited range of procedures under supervision. A licensed practical nurse has a one-year vocational course in nursing. They are qualified for more procedures and are responsible for communicating the patient's needs to medical staff. They are supervised by registered nurses and provide basic medical and nursing care. These nurses have to most contact with the patients and do most of the care.
A registered nurse has either an Associate of Science or Bachelor of Science in Nursing degree. They are qualified to make nursing diagnoses an to supervise certified and licensed nurses. An advanced registered nurse practitioner has postgraduate education in specialized aspects of nursing. These nurses include midwives, nurse practitioners, clinical nurse specialists and nurse anesthetists. A nurse practitioner is an advanced practise registered nurse. They are educated at graduate level and can practice independently. This was created so that nurses could be primary care providers.
A nurse can also earn a doctorate degree in two fields. In community projects and professional nursing academia, there is the Doctor of Nursing Practise. In the fundamentals and theory of nursing and research, there is the Doctorate in Philosophy.
In the United Kingdom, there are over 300 thousand nurses in a variety of settings and a range of specialties. To practise, all nurses must be registered with the Nursing and Midwifery Council.
Non-registered staff carry out a number of roles, often working in direct patient care. They must be supervised by a fully qualified registered nurse. A health assistant, also called nursing assistant, care assistant or clinical support worker, is au unregistered healthcare worker. Nursing associates focus on patient care, this job was introduced to reduce the growth in demand for registered nurses.
Most ward nurses are registered nurses with a completed university degree. Staff nurses, also called general nurses or staffers of nursing, are the first grade of qualified nursing staff. They have clinical duties for a set group of patients. Senior staff nurses, also called staffer managers, are more senior and experienced. Nurse practitioners carry out care at an advanced practise level, they commonly work in primary care.
The deputy ward manager (vrchní sestra), also called junior ward sister, or charge nurse, is responsible for the running of the ward and is responsible to the ward manager. The ward manager (staniční sestra), also called ward sister, charge nurse, nurse manager, or clinical ward nurse lead, is the nurse responsible for running a ward or unit and the administration. This nurse has budgetary control, employs staff, and is responsible for the local management. If there is a need to employ several nurses at a ward manager level, one of them acts as the senior ward manager, also calles senior ward sister or senior charge nurse.
There are also positions above the ward level. The clinical nurse manager, also called nurse lead, is responsible for an entire directorate or department, or alt least more than one ward. The nursing director, also called nurse matron or modern matron, is responsible for overseeing all nursing within a department or directorate.
Clinical nurse specialists and clinical nurse consultants specialize in a particular area, such as intensive care, and they have extensice specialist knowledge and experience. A clinical nurse specialist provides clinical leadership and education for staff nurses working in their department. A nurse consultant is a higher level of nurse specialist, they are also active in research and publication activities.
Ward rounds are regular visits paid by medical staff to hospital inpatients under their care, in order to review their progress. The doctors ask the patients questions and the nurses report their data. This helps the doctors to decide further treatment.
Rapid response teams, also called medical emergency teams, high acuity teams or critical care outreach team, are groups of designated hospital staff who quickly come to a patient's room if there is any indication that their condition is worsening. These teams often include a doctor, a nurse and a respiratory therapist. They are trained in early resuscitation interventions and advanced life support.
Allied health professionals are health care professionals that provide diagnostic, technical, therapeutic and support services in connection with healthcare.
A healthcare technician, also called patient care technician, helps nurses with care and provides basic procedures. A surgical technologist, also called a scrub or operating technician, works as a part of the team delivering surgical care. A medical technologist, also called a medical laboratory scientist, performs analyses of body fluids and works in clinical laboratories. A pharmacy technician performs pharmacy-related functions in collaboration with a pharmacist.
A midwife cares for mothers and newborns around childbirth. A lactation consultant specializes in the clinical management of breastfeeding.
A paramedic is a specialist who responds to emergency calls for medical help outside of a hospital. A psychologist helps to diagnose and solve patient's problems by providing counseling.
A physical therapist, also called a physiotherapist, helps to treat conditions and improve physical functions through rehabilitation. They help patients to adress mobility issues and educate about exercise. An occupational therapist helps patients recover by developing meaningful activities.
A ward orderly, also calleshospital porter or unlicensed assistive personnel, is a hospital attendant who assists staff, their duties are usually clasified ad routine tasks involving no risk for the patient. They can move equipment, furniture and patients around the hospital and take care of patient lifting and transport. A receptionist, also called a ward clerk, helps people with directions and makes arrangements, they are staffed at the ward reception desk.
History of Healthcare and Nursing
 The earliest documented institutions aiming to provide cures were ancient Egyptian temples. Institutions created specifically to care for the ill also appeared in ancient India. The earlies surviving encyclopedia of medicine is Charakasamhita written in Sanskrit, dated sometime from 100BC to AD150.
The earliest documented institutions aiming to provide cures were ancient Egyptian temples. Institutions created specifically to care for the ill also appeared in ancient India. The earlies surviving encyclopedia of medicine is Charakasamhita written in Sanskrit, dated sometime from 100BC to AD150.In Ancient Greece, temples dedicated to the healer-god Ascleius functioned as centres of medical advice and healing. The Romans constructed buildings called valetudinara for the care of sick slaves, gladiators and soldiers arond 100BC.
Christianity lead to an expansion of care and, following the First Council of Nicaea in AD 325, constructions of a hospitals in every cathedral town began. Hospital care was driven by Christian mercy and Byzantine innovation, which included specialized hospital staff. Their hospitals had the chief physician, professional nurses and the orderlies and by the 12th centrury, Constantinopole had two well-organised hospitals. Their doctors were both male and female and there were specialized wards and systematic treatment procedures.
During the Middle Ages, the rise of Christianty had a great effect on the practise of medicine. Christian monasteries became centres of accumulation of the medical knowledge and practise experience. Saint Benedict of Nursia was the founder of the Order of Saint Benedict, he established Monte Casino as the first monastery in Europe and the orded founded a hospital that is considered the first hospital in Europe of the new era.
Durind the 16th and 17th centuries, hospitals became secular institutions and in the 18th century voluntary hospital movement began. In 1710 in Berlin, Charité was founded as a response to an outbreak of plague. In 1765, the Royal Naval Hospital was opened, it was a pioneer of hospital design in having pavilions to minimize the spread of infection. In 1784 the Vienna General hospital was founded and became the world's biggest hospital.
Hospitals and medical staff became professionalised in the 19th century.
The earliest nurses may have been the attendants described in Ancient Greece in the 5th century BC. Around the same time in India, nurses were encouraged to study the human body. But before the foundation of modern nursing, members of religious orders, nuns and monks, often provided nursing-like care. The first known Christian nurse was Phoebe and she is mentioned in the Bible. Because of this, nurses are sometimes referred to as sisters in many countries.
In Europe, the Reformation was a major setback for the nursing professions, because monasteries and convents were closed. Professional nurses started training in the 19th century, with many women joining the Order of Exaltation of the Cross during the Crimean War. There were many important nurses, for example Florence Nightingale, Mary Seacole, Agnes Hunt, Agnes Jines, Linda Richards, Clarissa Harlowe Barton and Marianne Cope. Formal use of nurses in the modern mlitary began in 1880.
In the 20th century, nurses started to train in hospitals and the emphasis was on practical experience. For some time, nurses were seen as free labor and were commonly exploited. The profession changed during WWII, when nurses volunteered for service overseas.
The modern era standardized nursing education, with both undergraduate and postgraduate degrees. Nurses became recognized as a profession and an academic discipline. Today, it is considered a gender-neutral profession, although most nurses are still women.
Florence Nightingale was a British social reformer, a statistician and the founder of modern nursing. She became famous during the Crimean War, in which she served as a manager and trainer of nurses, she organized care for wounded soldiers. She became an icon of Victorian cultura and is known as the Lady with the Lamp because of her rounds at night.
Her social reforms included improving healthcare for all sections of British society. She advocated better hunger relief in India. She helped to abolish prostitution laws that were harsh for women and helped them to expand acceptable forms of participation in the workplace.
She hepled to restructure the modern hospital. She did extensive research and came to the conclusion that pavilion design hospitals have the best outsomes. She pioneered the modern profession of nursing. She was an example of compassion, comittment to patient care and dillegent and thoughtful hospital administration.
She helped to improve sanitation standards. She raised issues such as bad drainage, contaminated water, overcrowding and poor ventilation and how they are causing high death rate. She implemented hospital hygiene protocols that are common today and advocated for improving the patient experience.
She emphasized the importance of statistical measurement for determining the success rate of a given intervention. She also pushed for administrative reform at hospitals. She pioneered visual presentation of information and statistical graphics.
In 1860, she laid the fondation of professional nursing with the establishment of her nursing school, the Nightingale School and Home for Nurses, at Saint Thomas' Hospital in London. The mission of this school was to train nurses to work in hospitals and with the poor. She wrote about 200 books, pamphlets and articles and became an icon of English feminism.
In recognition of her work in nursing, the Nightingale Pledge is taken by new nurses and the Florence Nightingale Medal is the highest international distinction a nurse can achieve. The International Nurses Day is celebrated on her birthday, May 12.
Healthcare in Opava
Opava has a long history of healthcare, which is connected to several religious orders. Healthecare was provided in monasteries and later, since the 18th century, hospitals were founded for professional care.The Order of Brothers of the German House of Saint Mary in Jerusalem, commonly known as the Teutonic Order (Řád německých rytířů), came to Opava in 1204. This military order was founded in 1192 to aid Christians on their pilgrimages to the Holy Land and to establish hospitals. Its members were known as the Teutonic Knights and they were given posessions in Opava by Margrave Vladislav Jindřich and Duke Přemysl Otakar I. This order became the dominant power of healthcare in Opava and run the Hospital U rytířů since 1843. This order is still very rich and helped Opava after the 1997 floods.
The Order of Friars Minor Conventual, commonly known as the Conventual Franciscans or Minorites (Řád menších bratří konventuálů - monorité) was founded in 1209 by Francis of Assisi. Friars are called to live in service to society, they live in poverty as a mendicant order (žebravý řád). The Order came to the Czech Lands in the 13th century and founded a convent in Opava in 1234. In 1785, a parish (farnost) was established next to the Church of the Holy Spirit (svatého Ducha). Since the 19th century, a military hospital was a part of the complex.
The Order of Preachers, also known as the Dominican Order (Řád bratří kazatelů - dominikáni), came to Opava in 1291 and founded the Curch of Saint Václav. This mendicant (žebravý) order of preachers and teachers has an unlucky history connected to Opava. All his members died in 1542, when the plague hit Opava, the monastery burned down in 1556 and in 1585, an angry mob looted the monastery. In 1786, the monastery was closed due to financial problems.
The society of Jesus, simly called the Jesuits (Tovaryšstvo Ježíšovo - jezuité) is a religious order founded by Ingatius of Loyola in 1534. The society engages in evangelization and apostolic ministry and the jesuits were are famous in the field of education, research and cultural pursuits. The Jesuits came to Opava in 1625 and took ove the Church of Saint George from the Teutonic Order. Since 1630, they started a grammar school and since 1643, they changed the location to their own college. In 1655, the city gave the order property from the Ratibořská gate to the Church of Saint Adalbert (svatý Vojtěch).
The Congregation of the Sisters of Mercy Of the Third Order of Saint Francis (Kongregace milosrdných sester III. řádu svatého Františka) began in Opava as a communion in 1844. Since 1856, the sisters worked as nurses in hospitals and run an orphanage (sirotčinec). Since the end of the 19th century, there were over 500 sisters working in hospitals, asylums and other institutions, in 1912, the founded a nursing school (Řádová ošetřovatelstká škola).
The Congragation of the Daughters of Divine Charity (Kongregace dcer Božské lásky) was founded in Vienna in 1868 and came to Opava in 1870. The main aim was to provide work for poor girls, care for orphans and the elderly and education. In 1907, the Marianum was founded and it became a military hospital durong WWI. During WWII, the center of attention shifted to mentally ill children.
 A hospital is first mentioned in Opava in the 14th century, some were founded by religious orders and some by the city and its rich merchants.
A hospital is first mentioned in Opava in the 14th century, some were founded by religious orders and some by the city and its rich merchants.In 1443, the Hospital of Saint Anthony and in 1583 the Hospital near the Ratibořská gate were founded. In 1782 the Friedenthal Hospital was founded. In 1805, the Heidrich Institute was founded on Ostrožná Street, it included a pavilion for the mentally ill. The Teutonic Order founded the Hospital U rytířů in 1843. The first city hospital was founded in 1800 in a Franciscan monastery, but it was destroyed in 1805 after the Battle of Slavkov.
The care for mentally ill patients was always centred in Opava. In 1841, a new pavilion was built for the mentally ill in Heidrich Hospital, a big improvement from the previous prison-like accommodation. In 1773, an old castle in Město Albrechtice was renovated into an asylum. In 1889, a new asylum was built as the most modern in Central Europe, it has 200 beds which were not enough.
In 1894, a new hospital was planned with 12 pavlions for health departments and 3 for administration on Olomoucká Street. The construction began in 1898 and in 1900 the hospital was opened with the capacity of 273 beds. The original project was never finished. In 1944, the hospital was badly damaged and many people died, in 1945 it was evacuated. In 1996, the Silesian Hospital was founded and it also runs the Museum of Nursing and the Museum of Pathology. Today, the hospital has 650 beds and 1200 employees and the Psychiatric Hospital has 863 beds and about 6500 inpatients every year.









No comments:
Post a Comment